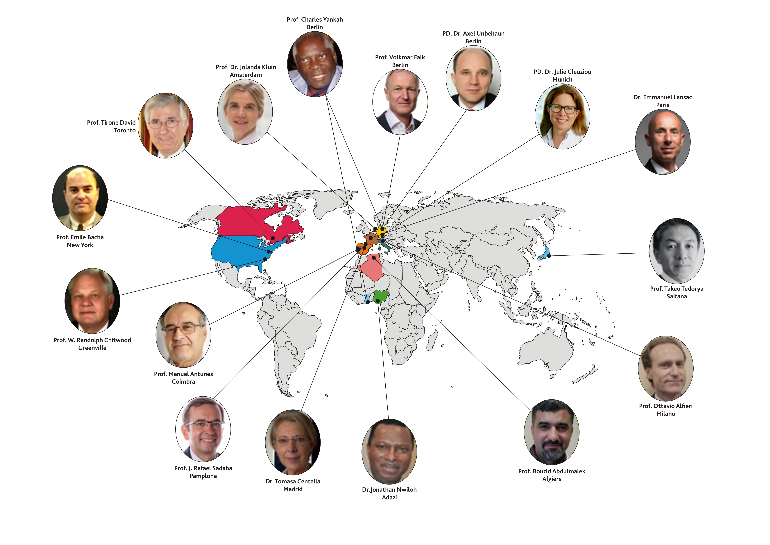
MESSAGES FROM FACULTY & WORLD HEART VALVE EXPERTS
History > Global Heart Valve Disease Day Webinar
| | | |  |
Messages to the Global Heart Valve Physicians & Patients | |
 Prof. Dr. Tirone E. David, Chair, Peter Munk Cardiac Centre, Toronto General Hosp. Canada | “The ideal heart valve substitute is yet to be developed and every effort should be made to repair, rather than replace diseased heart valves. This course promises to bring to you the state of art heart valve repair and when this is not feasible, the best alternative for replacement“ |
 Professor W. Randolph Chitwood Jr, MD FACS FRCS (England), Emeritus Professor and Chairman of the Department of Surgery. Emeritus Director and Founder East Carolina Heart Institute Chair East Carolina University, Brody SOM Greenville, NC | “Less Invasive mitral valve surgery has become a standard in many centers world-wide. The benefits with less blood loss and faster recovery are helpful to patients. The results have been shown to be safe and equal to conventional approaches. Also, mitral valve disease with concomitant atrial fibrillation should be treated at the same time.” |
Prof. Volkmar Falk, Medical Director, German Heart Centre & Director, Cardiothoracic & Vascular Surgery, German Heart Centre/Charité, Berlin, Germany | Minimally invasive mitral valve repair through a non-rib spreading right lateral mini-thoracotomy using femoro-femoral bypass and transthoracic aortic clamping is the standard of care for Carpentier type 2 degenerative mitral valve disease. Mortality in all comer population at the heart center in Berlin is less than 1% with a repair rate > 95%. The benefits of this procedure as compared to a standard sternotomy approach are shorter ventilation and hospitalization times, less need for blood products, and higher repair rates. The latter may result from a bias as this approach has been mainly adopted by high-volume centers with expertise in reconstructive valve surgery. A CT- angiography is recommended prior to surgery, to rule out peripheral artery and aortic disease. Severe mitral annular calcification is a relative contraindication, as decalcification can be difficult using endoscopic instruments. More than mild aortic insufficiency is another contraindication, as myocardial protection can be difficult. Age and body size (except for morbid obesity) are no limiting factors. Additional costs result from more expensive cannulas, the need for dedicated instruments and the use of 2D or 3D endoscopy. Modifications of the procedure may allow for a cost saving alternative. |
 | "Preservation of the native mitral valve is better than valve replacement in regard to outcome, quality of life and cost.The edge to edge technique, consisting of approximating the free edge of the leaflets at the point of regurgitation, is a valuable addition to the armamentarium for mitral valve repair. Furthermore, the edge to edge technique is the basis of the most widely used method of percutaneous correction of mitral regurgitation (MR).Although the edge to edge repair has been predominantly carried out in degenerative and functional MR, there are many situations of organic MR which can be conveniently treated with a stitch connecting the leaflets at the right point.This has to be taken into account by surgeons operating children with MR in whom valve replacement should be avoided." |
 | Training for expertise in heart valve surgery. It is compelling for paediatric cardiac surgeons to offer open repair procedures on faulty congenital and rheumatic heart valves to their young patients which allow uniform somatic growth of child’s own native valve, without life-long anticoagulation therapy. Children in LMICs with pure MS can even benefit from simple closed transatrial surgical valvotomy techniques than doing nothing, if interventional procedure, open repair are not available or affordable. Heart valve repair demands experienced surgeons and high volume institutions for achieving good results. Besides clinical learning, regular teaching programs on heart prototypes, biological simulators initiated by German Heart Centre Berlin in Ghana will enhance the skills of young surgeons in Africa to achieve competence that optimizes ‘‘ learning curve‘‘ results for repair of complex faulty congenital, rheumatic/inflammatory and degenerative heart valves under tutorial guidance. |
 Prof. Dr Manuel J Antunes Emeritus Professor Department of Cardiothoracic Surgery, Faculty of Medicine, University of Coimbra, Portugal | Despite some technical advances, rheumatic valve repair remains challenging. It requires experienced surgeons, but experience only comes with practice. Hence the encouragement for cardiac surgeons to learn and pursue mitral repair in these patients, having in mind the proven benefits by comparison with valve replacement. I have consistently received encouraging feedback from surgeons and residents who assisted to tutorials and wet labs or live operating room demonstrations, with positive impact on their own surgical activity. Some have initiated and maintained mitral valve repair programs where they did not exist before. |
 PD Dr. Julie Cleuziou, Deputy Director, Snr. Consultant Congenital & Paediatric Cardiac Surgeon, German Heart Centre Munich Munich, Germany | Valve surgery in the young is always involving the future of the patient. Growth is an important aspect, the need for exchange of biological valves and the necessity of anticoagulation therapy in mechanical valve prostheses are features which need to be addressed in these patients. The patient’s own valve is always the best option in growing children. |
 Dr Emmanuel Lansac, Chirurgie Cardiaque, Institut Mutualiste Montsouris, Paris, France | As recommended by lastest EACTS/ESC guidelines, we should try to repair any regurgitant valve. Bicuspid AI are excellent candiate for Valve repair but do forget Rheumatic AI particularly if the annulus is dilated (>25 mm). Standardisaton of repair can be achieved with valve resuspension/reconstruction with double sub and supra valvular annuloplasty restoring the ratio annulus/STJ. |
 | |
 PD. Dr. Axel Unbehaun, Consultant Cardiac Surgeon, German Heart Centre Berlin/Charité Berlin, Germany | The bicuspid aortic valve (BAV) is no longer no target for TAVI. Surgeons should stay involved. Don‘t try to stop the trend. BAV is a heterogeneous pathology. A calcified raphe together with an excess leaflet calcification are predictors of poor outcome after TAVI. All other forms can already be treated with good results. The strategy planning process must take into account the different forms of BAV. New simulation tools are helpful to predict the post-procedural result precisely. Randomized trials (SAVR vs. TAVI) and monitored long-term observations are lacking, especially to assess the incidence of structural valve deterioration, thrombosis and endocarditis. |
 Prof. Takeo Tedoriya, Director, Cardiovascular Center, Ageo Central General Hospital Ageo, Saitama, Japan | Ozaki procedure vs. Ross procedure Although Ozaki procedure should be one of reliable leaflet reconstruction procedures using autologous pericardium, durability might be uncertain. We have relatively many redo-AVR after Ozaki procedures due to torn of commissure sites as well as infective endocarditis. Also, when you have unbalanced Valsalva cases such as bicuspid AV, Ozaki procedure might be not suitable fashion because theoretically leaflet size should be decided cusp-attachment lines. In such cases, you have to select a bit longer leaflet resulting fluttering of tips of leaflets and distortion of the leaflet coaptation line. Our procedure is based on CARVER procedure of Prof. Song, which allows three same-sized leaflet reconstruction. We have modified the original procedures, to obtain at least 4mm coaptation height, to secure appropriate stitching zone and double stitching of commissure site to reinforce this most stressful regions, and to make adjustment procedures by evaluation of the aortic root preoperatively by 3D-hologram VR imaging. According to our limited experience, our procedure would be useful in selective cases with excellent hemodynamic performance and no fluttering nor distortion of leaflets, which might meet with better durability of this reconstructed valve, although our longest follow-up period is still 5 years. Of course, strict follow up should be indispensable to clarify our wishful prediction. |
 Prof. Abdelmalek Bouzid, Pediatric & Adult Cardiac surgeon University of Algiers 1 Faculty of Medicine, Algiers, Algeria | Heart valve diseases remain a main problem of public health in many countries in the world. Rheumatic heart disease is still a concern in low and medium income countries. The challenge is how to achieve the best quality of life if possible and not only a survival. This main goal as a guide, is to have a personalized decision for every case, close discussion with patients is mandatory to have the best results, the socioeconomic status and the level of education of these patients allow us to choose different approaches. Valve repair is the ideal choice for preserving the native valve as longer as possible since it's function is preserved and it allows a normal quality of life, however this goal is not always possible to achieve. In such cases the choice of the valvular substitute depends on multiple factors: the socioeconomic status and educational level of the patients; age, affordability for the price and access to different valve substitutes. The ideal choice of valve replacement is a prosthesis that doesn't require any anticoagulant treatment, has excellent hemodynamic profile and very long durability. Biological prosthesis is preferable in elder patients which is problematic in younger population because of the need for many reoperations in their life times. The benefit/risk balance of the choice of biological versus mechanical prosthesis must be discussed and assessed for each case according to the wish of the patient, his professional requirements, the possibility to have a close control of the anticoagulant treatment and the quality of prosthesis affordable. |
 Jonathan O. Nwiloh Dr. Joe Nwiloh Heart Center, St. Joseph Hospital, Adazi, Nnukwu Anambra State, Nigeria | Although Rheumatic heart disease (RHD) remains the leading cause for heart valve surgery especially in adolescence in sub-Saharan Africa (SSA), an increasing number of adults are been diagnosed with non-rheumatic valvular heart disease with the wider availability of echocardiography over the last 1 – 2 decades. These degenerative valve diseases involve aortic & mitral valves but more often the mitral resulting in chronic primary mitral regurgitation. Chronic secondary mitral regurgitation is also increasingly seen in some patients with nonischemic cardiomyopathy mostly from hypertension and ischemic cardiomyopathy. Unfortunately, most patients in SSA present late with symptomatic severe mitral regurgitation (Stage D), severe heart dysfunction and prohibitive surgical risk. Even when able to successfully undergo surgery, they have a late excess mortality. Improving long term survival will require better patient education by the treating physicians on the life-threatening nature of their condition even if initially asymptomatic, emphasizing the importance for close monitoring to detect onset of heart dysfunction to enable early referral for appropriate intervention before development of irreversible heart damage. Since hypertension is the leading cause of heart failure in SSA, patients also need counselling on antihypertensive medications compliance to decrease the incidence of chronic secondary mitral regurgitation from heart failure remodeling. Because most patients cannot afford a redo heart surgery due to financial constraints, we prefer mechanical valve replacement if there are no contraindications to long term anticoagulation in patients less than 60 years. Valve repairs are reserved for uncomplicated rheumatic and degenerative mitral valves with high chances of success for a durable repair. |
 Prof. J. Rafael Sádaba, EACTS Interim Secretary General Snr. Consultant, Dept of Cardiac Surgery Complejo Hospitalario de Navarra, Lead clinician in the “Translational Cardiology Research Group” at Navarra Biomed Fundation Pamplona, Spain | "Mitral valve repair is already a well-established and standardised procedure which has been shown to have advantages over mitral valve replacement. Repair of the aortic valve and root also offers advantages over replacement, and it is following a similar path to that of mitral valve repair. Although the techniques available for aortic valve repair are perceived as being more demanding, the efforts by leading surgeons to standardise the techniques are yielding good results. I applaud the efforts to increase the awareness of heart valve disease among health care professionals and the promotion of repair techniques among surgeons." |
 Prof. Jolanda Kluin, Snr. Consultant Cardiac Surgeon, Director, Translational Cardiothoracic Surgery, Amsterdam Univ Medical Centre, The Netherlands | On this Global Heart Valve Disease Awareness Day this digital meeting brings together expert colleagues from around the world to discuss the state of the art in heart valve disease treatment. By joining the meeting you will be part of this community. Only together we can ensure the best treatment for every patient with heart valve disease |
 PD. Dr Regina Bokenkamp, Snr. Consultant Congenital & Paediatric Cardiologist and Interventional Cardiologist, Leiden Univ Medical Cenntre, Leiden, The Netherlands | Percutaneous and surgical techniques for
pulmonary valve replacement should be seen as complementary tools and not as
competing techniques. The collaboration between cardiologist, interventionalist
and surgeon is essential to find the best solution for the individual patient. |
 Prof. Charles Yankah, Cardiothoracic & Vascular Surgeon, CEO, Founder, Global Heart Forum, German Heart Centre/Charité Berlin, President, PASCaTS, Berlin, Germany | Charity heart teams have responded to the emergency call of low and middle income countries (LMICs) to provide cardiac valvular surgery to the underserved communities esp. the paediatric population. The charity surgeons are confronted with high demand for primary valve repair in the management of congenital and rheumatic heart valve diseases. Late presentations with valvular endocarditis complicated by burrowing abscess formation requires complex surgical reconstructive techniques and valve replacement, a challenging procedure even for experienced surgeons. Rescue procedure is warranted in most cases. Although mechanical valves are preferred in young population, biological valves; stented and stentless xenografts including decellularized homografts are alternatives. |
Global Heart Valve Disease Awareness | |
 Prof. Charles Yankah, Cardiothoracic & Vascular Surgeon, CEO, Founder, Global Heart Forum, German Heart Centre/Charité Berlin, President, PASCaTS, Berlin, Germany | Rheumatic heart valve disease (RHVD) affect mostly the mitral valve (incidence: 85%: mitral stenosis, 10% (MS), mitral regurge, 75% (MR)) and aortic valve (incidence: 15%) among school age children and in adolescents. Prevalence of rheumatic MS among school children in sub-Saharan Africa is 12-15%. RHVD can present as a mixed mitral lesion (MS+MR). Fortunately, the incidence of RHVD has decreased by 8.67% between 1990 and 2017 while the degenerative heart valve disease has increased by 45% (Eur Heart J. 2003;24:1231-43, N Engl J Med 2007;357:470-6), 12-15% (sub-Saharan Africa, Yankah et al. 2020, J Chen et al.J Global Health 2020). The untreated or advanced rheumatic mitral valve stenosis and regurge cause arrhythmias, heart failure, disabilities and premature death. Although the disease is preventable and surgically reparable most of the victims who live in resource limited regions have no access to this surgical treatment. Primary open surgical repair remains the concept, however, children with pure MS can even benefit from simple closed transatrial surgical valvotomy techniques if interventional procedure, open repair are not available or affordable. |
 Prof. Charles Yankah, Cardiothoracic & Vascular Surgeon, CEO, Founder, Global Heart Forum, German Heart Centre/Charité Berlin, President, PASCaTS, Berlin, Germany | Heart valve infection (endocarditis) is a serious life-threatening and fatal health condition. Untreated streptococcal throat infection will develop rheumatic fever which is the major cause of rheumatic heart valve disease (endocarditis, myocarditis, pericarditis). The toxins produced by the bacteria into the blood circulation attack and damage one or more heart valves (mostly the aortic or mitral valves). Heart valve infection (endocarditis) can also develop directly by bacteria or fungi which enters into the blood circulation (bacteraemia) from several sources. Vulnerable individuals with weak immune system or under immunosuppressant therapy are susceptible for developing blood infection (baceteraemia and sepsis- inflammatory immune response triggered by an infection). The other risk factors include rheumatic, congenital and degenerative valve lesions, intracardiac prosthetic material, intravenous drug use, and healthcare contact. The sources of blood infection are soiled traumatic wounds, major and minor surgical procedures (dental extraction, gastroenterological procedures (gastro-coloscopy), genitourinary procedures etc.) without antibiotic protection. Bacterial or fungal blood infection (bacteraemia) which directly attacks one or two heart valves (endocarditis) can develop serious life-threatening health conditions such as sepsis, irreversible damage of the heart valve, multiorgan failure and death. Consult your house physician if you are suffering from sore throat with fever, chest and joint pains (migrating polyarthritis) etc for examination and treatment. The diagnosis and treatment are based on a multidisciplinairy team approach consisting of effective antimicrobial therapy and surgery if conservative therapy fails within three weeks (uncontrolled infection) or serious cardiac structural damage occurs suddenly (mobile vegetation imminent of embolization, abscess and fistula formation, acute valve tears or holes, prosthetic valve detachment leading to acute regurge and acute heart failure. Prevention of heart valve infection is therefore better than medical/surgical therapy. This message is a wake up call to global cardiovascular community and civil society. Education is the key for prevention of heart valve infection (endocarditis). Regular washing of hands, daily tooth brushing with tap or boiled water, antibiotic treatment of febrile sore throat are the most cost effective health measure against rheumatic heart valve infection (endocarditis). Extracardiac complications include septic embolism- spread of dislodged infected blood clots to the brain, spleen, extremities, intestines, mycotic aneurysm, and vertebral osteomyelitis. Antibiotic prophylaxis against febrile throat infection, soiled traumatic wounds, antibiotic treatment of clinically manifested blood infection (sepsis) surgical removal and replacement of the infected heart valve can save lives. |
 Prof. Charles Yankah, Cardiothoracic & Vascular Surgeon, CEO, Founder, Global Heart Forum, German Heart Centre/Charité Berlin, President, PASCaTS, Berlin, Germany | Surgical Treatment of Heart Valve Disease There are three major types of valve procedures: 1. native valve repair (Carpentier mitral valve technique, deVega tricuspid valve technique, Kay/Wooler plasty, Paneth/Burr posterior mitral annuloplasty, Duran aortic and Acar mitral cusp augmentation, Ozaki aortic cusp reconstruction etc.) 2. valve retention/sparing (aortic root remodeling technique Yacoub, Yacoub/Lansac technique and reimplantation technique David) and 3. replacement. Valve replacement can be biological tissue 1. Autograft (patient’s own pulmonary valve transplanted to replace the diseased aortic valve- the Ross operation), 2. Homograft (aortic or pulmonary valve from a donor to replace the diseased aortic valve of the same species- the Ross/Barratt-Boyes subcoronary implantation, Ross complete aortic root replacement) or 3. Xenograft (stented and stentless: tissue valve from a donor of different species -bovine or porcine to replace the diseased valve of a different species- human) or 4. mechanical (artificial- requires life-long anticoagulation (blood thinner) therapy). The choice of procedure and valve prosthesis depends on patient’s clinical data, diagnosis, technical considerations, and surgeon’s preferences. Anticalcification treated stentless bioprostheses are readily available in various sizes, technically easier to implant and more durable due to anticalcification treatment. The homograft and stentless xenograft valves demonstrate equal hemodynamic characteristics. It is evident that the rate of homograft and xenograft valve failure in young patients increases after 10 years compared with mechanical valves. Reoperation for calcific structural valve deterioration (SVD) is more challenging than stentless xenograft reoperation. Currently, decellularized homografts and tissue engineered pulmonary and aortic valves as biological compatible tissues are conceptually used clinically for endogenic recellularization and regeneration for improving their durability. Early results indicate a light at the end the tunnel. Repair of heart valves (aortic, pulmonary and mitral or tricuspid) in children is most preferable procedure if the valve tissue is not irreversibly damaged, for allowing uniform somatic growth of child’s own native valve, without life-long anticoagulation therapy (blood thinning). If valve repair or reconstruction is not feasible In the aortic position in young patients, the pulmonary autograft operation, (the Ross operation) is an option. Yet, there are challenges in availability of valve repair or Ross operation experts in some centres in low and middle countries. In rheumatic fever endemic regions Ross operation is not a good option. It is compelling for paediatric cardiac surgeons practicing in LMICs to provide their young patients with native valve retention/ repair procedures before considering mechanical valve replacement. Meta-analysis of publications has shown that mechanical heart valve has potential valve-related morbidities such as thrombosis, bleeding, ischemic strokes which can be fatal. They are significantly higher in women of child bearing age in low and middle income countries (LMICs) associated with frequent hospitalizations. Prenatal counseling and clinical evaluation during pregnancies for women with mechanical heart valves is therefore highly recommended. The morbidities and negative quality of life favour application of 1. valve repair procedure as a first choice and 2. mechanical valve as a second choice of valve replacement. The third strategy for valve redo or replacement depends on the socioeconomic factors: affordability for anticoagulation drugs, compliance to INR monitoring, age and valve size at first reoperation for replacing mechanical valve with stented bioprosthetic valve at the age < 40-59 years. At the subsequent re-reoperation for SVD the age groups < 60-70 or > 70 years will benefit from transaortic valve implantation (TAVI). Extension of TAVI into younger age groups < 70 years with intermediate risk is likely to be preferred procedure. Factors for consideration are size of native valve, probability for early failure and risk for reoperation, Young patients undergoing, first bioprosthetic valve implantation requires aortic root enlargement procedures for accommodating 23-25mm valve to allow future TAVI if a redo bioprpsthetic valve replacement is required. Who benefits from valve repair procedures and bioprosthetic valve replacement? Sport men and women, women of child-bearing age, the elderly, professionals with risk of physical injuries, patients with dementia and Parkinson diseases, frequent globe trotters, contraindication for anticoagulation (haemophilia), uncontrolled hypertension etc.). |